Introducing Tunnelled CVAD (Central Venous Access Device)
CVADs come in a wide array of devices, each uniquely designed to meet specific needs. In essence, they all share a common feature: a thin, elongated plastic tube known as a “line” or “catheter.”
Imagine one end of this catheter comfortably resting in the body’s largest vein, the Superior Vena Cava. This vital vessel carries blood from the head, chest, and arms back into the heart. The other end of the catheter links to a device, seamlessly facilitating the injection of medications.
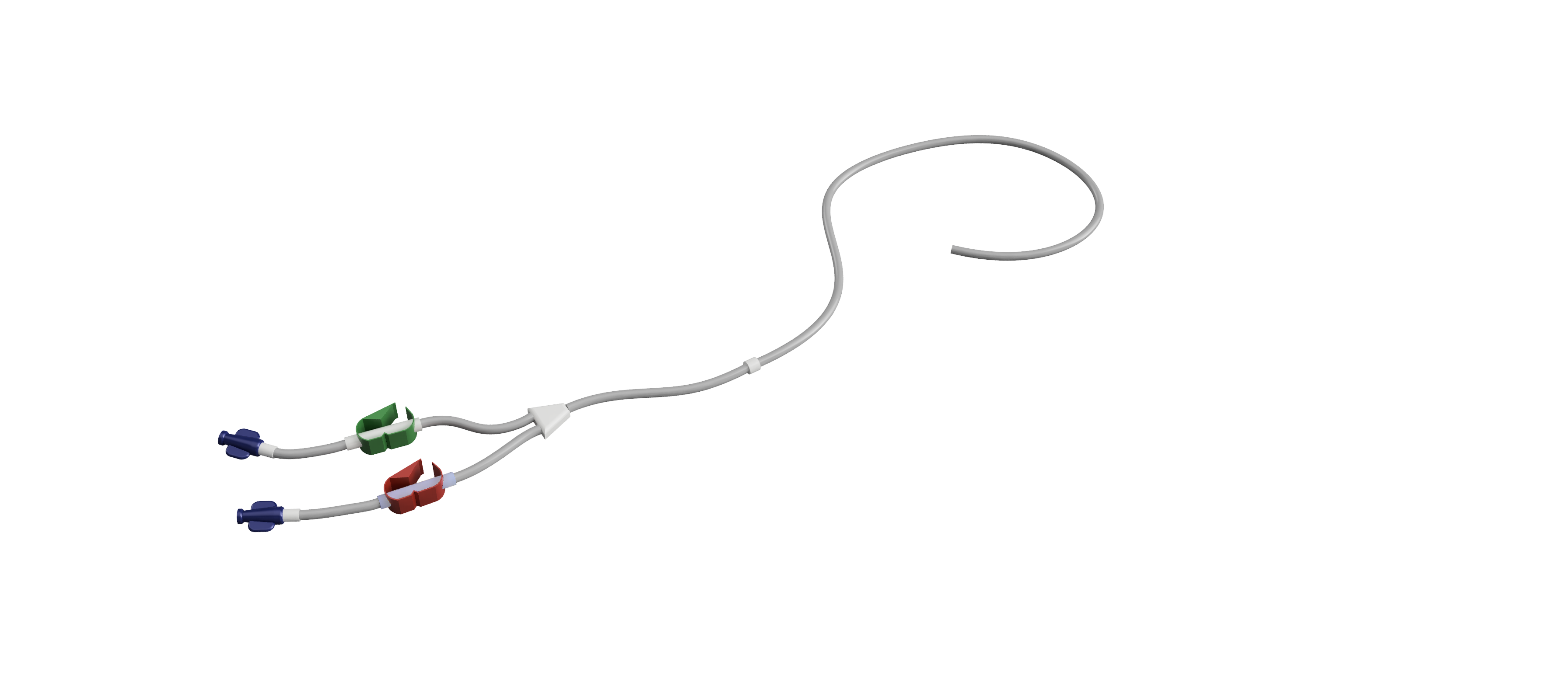
With a tunnelled CVAD the catheter emerges through a small scar on the front of the chest, culminating in a connector that serves as the access point for medication administration. A small “cuff” is embedded onto the line and secures the catheter snugly beneath the skin, ensuring the device remains firmly in position. Various types of Tunnelled CVADs exist, each possessing unique characteristics. The primary distinction lies in the number of lumens, with a Broviac® line featuring a single lumen and a Hickman® line accommodating two lumens, enabling the simultaneous administration of multiple agents.
Why Choose a Tunnelled CVAD?
When considering your options for central venous access, it’s essential to compare tunnelled CVADs and Portacaths. While the indications for both are similar, they have distinct characteristics that should be carefully weighed. Notably, tunnelled CVADs have a significant external portion that requires meticulous support, securing, and cleaning. However, one key advantage is their ease of access, with most nurses and healthcare professionals comfortable utilising them. In contrast, accessing Portacaths may require additional training, underscoring the importance of consulting with your healthcare team.
While the indications overlap, tunnelled CVADs are particularly useful where daily access is required in particular for delivering nutrition support directly into veins, known as ‘parenteral nutrition’ or PN. Other reasons to consider a tunnelled CVAD include:
Long-Term IV Therapy: Tunnelled CVADs are well-suited for patients requiring prolonged or recurrent intravenous therapy, such as chemotherapy, antibiotic treatment, or other medications.
Frequent Blood Tests: If you need frequent blood tests, a tunnelled CVAD simplifies the process by providing a dedicated access point, minimizing discomfort associated with repeated peripheral venipuncture.
Limited Peripheral Vein Access: Individuals with limited or compromised peripheral veins, often due to previous treatments, medical conditions, or surgeries, may find a tunnelled CVAD beneficial. It provides access to larger central veins, facilitating the administration of medications or therapies.
Extended Treatment Periods: If your treatment plan involves an extended period of therapy, a tunnelled CVAD can provide durable and convenient access, ensuring ease throughout the treatment duration.
Simultaneous Administration of Medications: Some tunnelled CVADs, like the Hickman® Line, have multiple lumens, allowing for the simultaneous administration of different medications or therapies. This feature enhances treatment flexibility and efficiency.
In making your choice, it’s crucial to consult with your healthcare team, considering your specific medical needs and treatment goals. The decision will be tailored to provide optimal care and convenience based on your unique circumstances.
How is the fitting process conducted?
The insertion takes place in sterile radiology operating theatres, employing local anaesthesia to ensure complete numbness in the targeted area, rendering the procedure painless. Although mild pressure sensations may be briefly felt, these are of short duration. Sedation is an option for all patients upon request to enhance the overall experience.
Both Ultrasound and X-rays are utilised in tandem to visualise the veins and the device, ensuring precise placement of each catheter at the chosen location. A minor scar of approximately 0.5cm is typical at the point of vein access, either just beneath or above the collarbone, depending on the selected vein. Additionally, there is a small 1cm scar used to bring the catheter out of the skin on the front of the chest. All incisions are closed using fully absorbable stitches or glue, eliminating the need for suture removal at a later date.
Typically, the entire procedure lasts between 20-30 minutes, with most patients ready to leave about 60 minutes after completion. If sedation is administered, the recovery period may be slightly extended, and it is imperative that someone drives you home afterward.
Where is the tunnelled CVAD positioned?
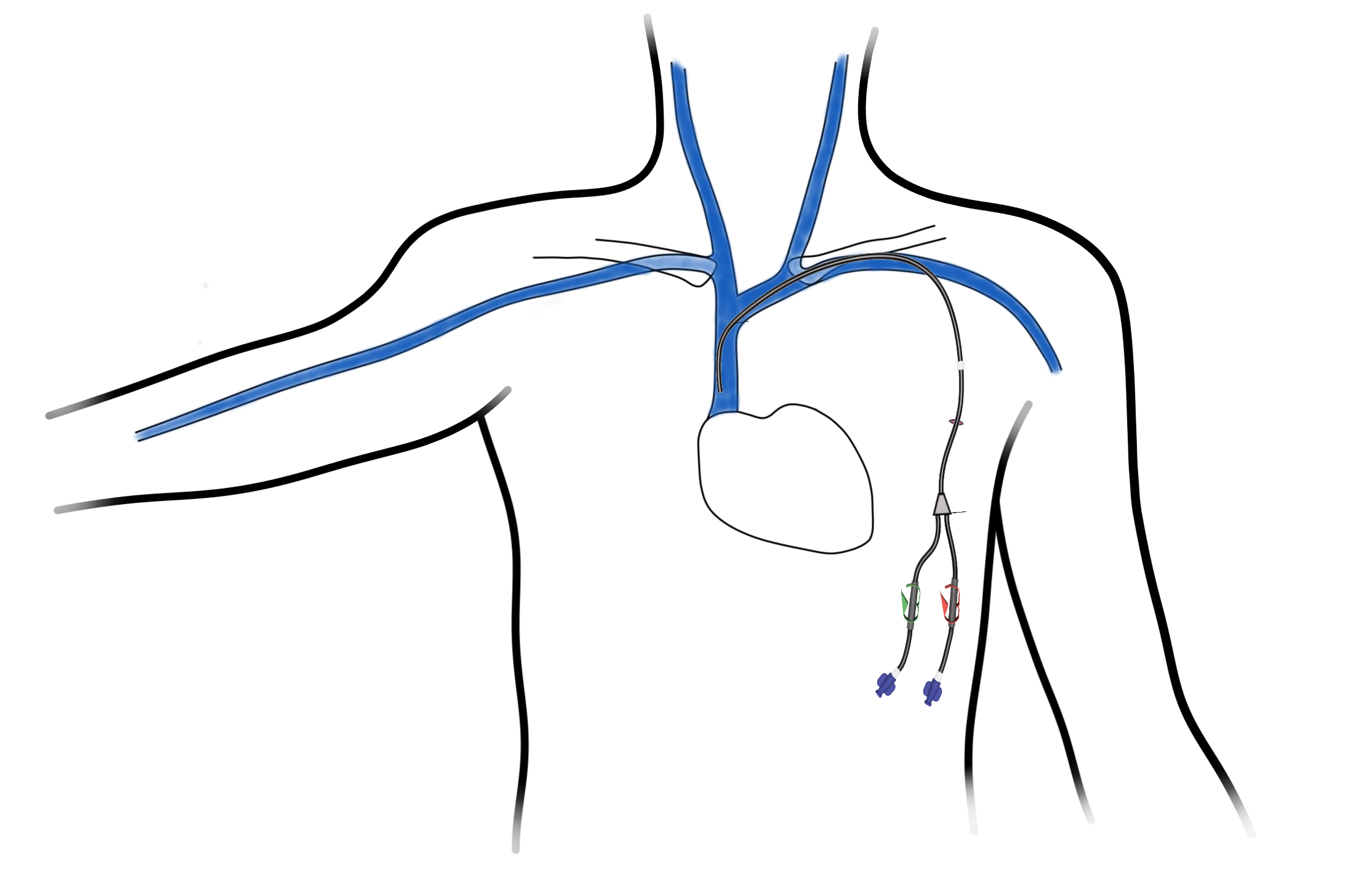
Tunnelled CVADs are typically situated on the chest, with the exact position being relatively flexible. Before the fitting procedure, Dr. Simpson will engage in a discussion with you, marking the precise location for the exit and external portion based on factors such as clothing preferences and undergarments, taking care to avoid interference with straps from bras, backpacks or seatbelts.
How Are CVADs Utilised?
CVADs are easily accessed thanks to the universal connectors at the catheter’s end. After ensuring the device is meticulously cleaned, a standard syringe can be effortlessly connected. Typically, the catheter is aspirated, drawing back a small amount of blood to ensure it is unobstructed. Subsequently, medications can be administered either through a syringe or an infusion pump.
Post-procedural Care Recommendations:
As a part of the CVAD extends outside the body, it’s crucial to take precautions to prevent accidental dislodging. A small cuff attached to the catheter becomes securely embedded under the skin after approximately 2 weeks, preventing catheter migration. While Dr. Simpson ensures a secure stitching underneath the skin during the initial 2 weeks, it is essential to be vigilant in safeguarding the device from potential snagging.
During the first 7 days, it is advisable to limit straining and strenuous activities to facilitate proper healing of the small scars and minimize bruising. Complete soaking of the area should be avoided, and showers can be taken by standing to the side and carefully washing around the site. When drying, use a gentle dabbing motion with a towel instead of rubbing. While most sports can be resumed after 14 days, it is advisable to refrain from contact sports and swimming for the duration the tunnelled CVAD is in place.
The local anaesthetic provides numbness for a few hours post-procedure, and any subsequent mild discomfort or pain can be managed with common painkillers such as Paracetamol and Ibuprofen. Many individuals report a dull ache at the site, collarbone, or neck area for a few days until the swelling and inflammation subside.
To maintain the continued functionality of the tunnelled CVAD, a monthly flush with saline is recommended. If your treatment schedule is more frequent, flushing will coincide with your sessions. When the device is no longer needed, removal involves a small scar above the securing cuff, and the tunnelled CVAD is easily extracted. This typically takes 5-10 minutes and is performed under local anaesthesia.
Reassurance Regarding Possible Complications:
While no medical procedure is entirely without risk, Dr. Simpson will thoroughly discuss specific concerns during the consent process. Rest assured, every precaution will be taken to prioritise your safety and minimise any potential delays in your treatment.
It’s important to note that bruising around the site is a common occurrence, especially if you are taking medications to ‘thin’ your blood but can be minimised by limiting activity in the first 48hrs.
Though there is a small risk of a blood clot forming around the catheter inside the vein, causing occasional swelling in the arm, such occurrences are rare. In this unlikely event, and if the tunnelled CVAD is still functioning, a cautious approach involves starting blood-thinning injections. Removal of the device becomes necessary only in the rarest of cases, allowing the clot to be naturally reabsorbed.
While complications such as device failure, infection, or damage to other structures (such as nerves or the lung) are exceedingly rare, it’s essential to emphasize that thorough measures are in place to address and mitigate these possibilities. Your well-being and the success of your treatment remain our utmost priorities throughout this process.
OPENING HOURS
| Monday | 14:00 – 20:00 |
| Tuesday | 18:00 – 20:00 |
| Wednesday | 18:00 – 20:00 |
| Friday | 14:00 – 20:00 |
OFFICE LOCATIONS